Heart failure is a chronic, progressive disease in which the heart becomes less able to pump enough blood to meet the body’s needs. In this sense, the heart muscle cannot sustain its workload; at the beginning of this condition, the heart tries to compensate this deficiency in some way, but over time it weakens and loses the ability to contract normally.
As a result, the heart muscle does not have the ability to pump enough blood into the circulation forcefully (systolic dysfunction), or it loses its ability to relax normally and may not fill properly during the rest period between beats (diastolic dysfunction) The body’s reaction to insufficient heart function causes fluid to accumulate (edema) in the lungs and tissues.
How can heart failure occur?
The heart receives venous (oxygen-poor) blood from the periphery (through the right atrium and right ventricle), favoring oxygenation by pumping it into the pulmonary circulation, then through the left atrium and left ventricle, pumping oxygenated blood into the aorta and then into the arteries for transport to all organs and tissues of the body. It is therefore possible, in a first approximation, to differentiate between:
- Systolic decompensation, in the presence of a reduced ability of the left ventricle to deliver blood
- Diastolic decompensation, in the presence of impaired left ventricular filling
In a routine check-up of left ventricular function, the left ventricle is commonly assessed by the so-called ejection fraction (percentage of blood that is pumped to the aorta with each contraction (systole) of the left ventricle), usually calculated by echocardiography, a more accurate distinction between the following:
- Decompensation of preserved (or diastolic) ejection fraction, in which the ejection fraction is greater than 50%
- Decompensation of reduced (or systolic) ejection fraction, in which the ejection fraction is less than 40%
- Slightly reduced ejection fraction decompensation, in which the ejection fraction is between 40 and 49%
This classification is important for the development of increasingly specific therapies, although currently there are only proven therapies for decompensation of reduced ejection fraction. In any case, echocardiographic studies are essential to make a timely diagnosis of this health condition and to follow up the treatment suggested by the cardiologist to the patient.
What tests should be done to make the diagnosis of heart failure?
To make the diagnosis of heart failure, tests should include a history (this includes collecting information about the person’s medical history and symptoms) and a preliminary physical examination. Subsequently, the treating physician may request some additional tests consisting of bioanalysis studies and instrumental tests, among which can be highlighted:
- Electrocardiogram
- Echocardiogram
- Cardiac magnetic resonance imaging, with contrast application
- Specific tests for blood levels of natriuretic peptides (substances produced mainly by the left ventricle; decompensation is ruled out when levels are within expectations)
- More invasive tests, such as cardiac catheterization and coronary angiography, are also possible
The electrocardiogram in most patients with decompensation may signal a left bundle branch block, an alteration in the propagation of the electrical impulse that can have effects on the mechanics of the heart, resulting in desynchrony of contraction and, consequently, a decline in cardiac contractile activity.
What is the treatment for heart failure?
Heart failure is a chronic disease that, in order to be treated, requires a multidisciplinary action to decrease symptoms, stop the evolution of the disease, reduce hospitalizations and increase patient survival, and simultaneously improving their quality of life. The main treatment options are:
- Lifestyle changes, including: decreasing salt intake, exercising aerobically and regularly, controlling fluid intake, and monitoring the diet to avoid weight gain
- Drug therapy may include inhibitors of the renin-angiotensin-aldosterone system and antialdosterone drugs. Beta-blockers and neprilysin and sodium-glucose co-transporter inhibitors may also be needed
- Cardiac resynchronization therapy with implantation of electrical devices such as pacemakers or defibrillators
- Open-heart operations
In addition to the early diagnosis and the different treatment options available, the active role of the patient and the collaboration between the multidisciplinary team and the treating physician are valuable. In that sense, medication and surgical options will be useless if the patient does not become aware of his condition and is not part of the solution to the problem that afflicts him.
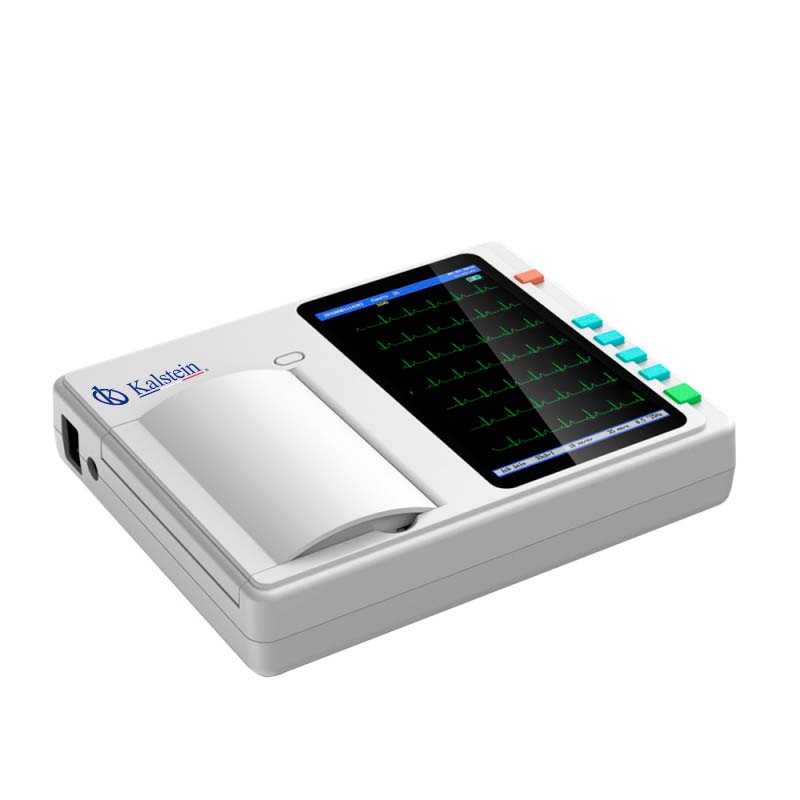
Kalstein electrocardiographs for detecting heart failure
Cardiologists require instruments with which they can make accurate diagnoses of different diseases, such as heart failure, which can be revealed with the use of an electrocardiograph. In that sense, the equipment manufacturer Kalstein has state-of-the-art 12-channel 12-lead electrocardiographs, touch screen, low noise and with thermal printing system of the electrocardiogram. For more details such as prices, purchase or quote check the link HERE or the link HERE